July 21, 2025
8 mins
Alpana Jha
July 14, 2025
8 mins
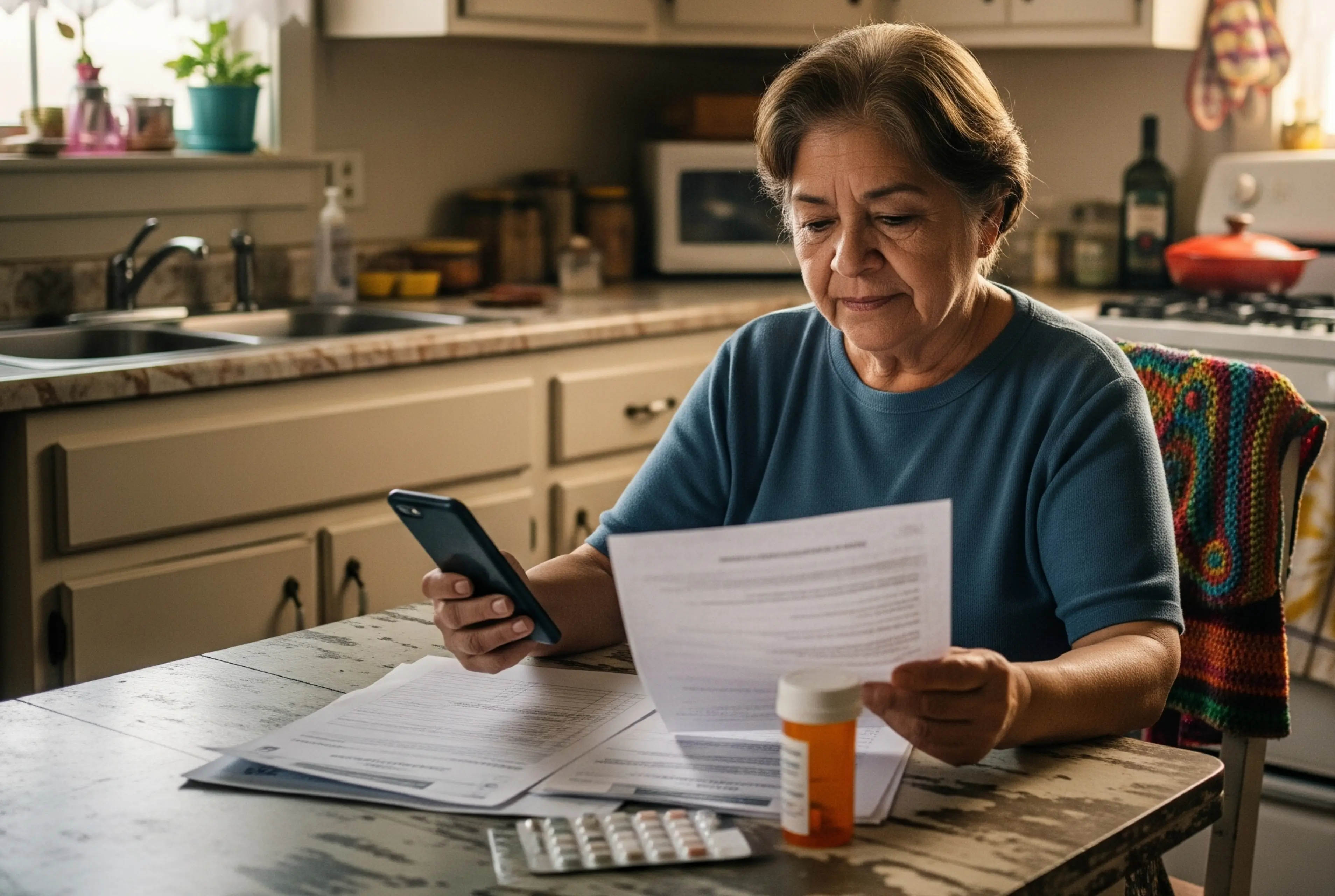
Health plans know member engagement is important. They invest in mailers, digital campaigns, and outbound calls- especially during high-stakes windows like AEP. But the thing is, members needs do not wait for open enrollment. They reach out when something is not working, and they expect answers right then.
When they have a question about a denied claim.
When they are unsure what their plan covers.
When they are discharged from the hospital and do not know what comes next.
They’re the ones that determine whether a member uses their benefits, stays with your plan, or leaves.
Why are members disengaging in the first place?
Because too often, members ask for help and don’t get it.
Members don’t disengage because they’re disinterested. They disengage because they’re worn out- from long hold times, unclear benefits, and systems that expect them to figure it out alone. When help is delayed, scattered, or too hard to access, it creates friction. And friction leads to frustration.
Traditional engagement strategies often center on outbound volume. But what members need is timely, accurate, and understandable help when they are already navigating the complexity of care. The problem isn’t always awareness, it’s accessibility. They know they have benefits. They just can’t use them easily.
This gap- between the promise of support and the reality of the experience, is what causes members to pull away.
It’s not a lack of communication. It’s a lack of connection, at the moment it’s most needed.
How does timely support improve member engagement?
When support comes at the right time, it lowers the barrier to action. Members don’t get stuck. They don’t abandon their care or let things slide. They get clear, useful directions at the exact point of need.
Timely support isn’t just helpful. It’s what earns attention and trust in a crowded, noisy system. And over time, it leads to better outcomes, not just for the members but for the plan too.
Organizations using real-time, voice-enabled tools have seen:
These numbers point to a shift that’s already underway; real-time support is quickly becoming the expectation.
Health plans that don’t adapt risk falling behind- not just in member satisfaction, but in operational efficiency and retention outcomes. What was once a competitive edge is now becoming table stakes. As expectations rise, delayed responses and impersonal service feel increasingly out of step. Timely, human-centered support is no longer a differentiator; it’s the bare minimum.
What happens when members don’t receive timely support?
Every time a member struggles to get an answer, there’s a downstream cost.
They might skip preventive care.
They might delay the treatment.
They might call your service team multiple times or stop calling altogether.
Eventually, they leave.
The average Medicare Advantage plan loses over $60 million per year to voluntary disenrollments, and it can cost up to $500 to acquire each new member.
Churn also impacts CMS Star Ratings and bonus payments. And those who leave don’t do so quietly- poor word-of-mouth spreads fast, especially in competitive markets.
What does real-time support actually look like?
According to HealthEdge, 60% of members report higher satisfaction when they receive timely support. That stat isn’t just about experience scores; it reflects a deeper need for responsiveness. Members want to feel heard for the first time. They want support when it matters-while they’re still at the pharmacy, still on the phone, still reading the letter that didn’t make sense. And when they get that kind of support, it shapes how they see your plan going forward.
This kind of support changes how members behave and what they believe about your plan. Members who feel supported are more likely to follow through on care, ask questions early, and stay engaged throughout the year. Timely support reduces abandonment, minimizes confusion, and improves first-call resolution. And in a market where small delays lead to big consequences, that kind of responsiveness becomes a powerful retention tool.
How does Mia make this possible?
Mia is AI-powered, voice-first, member retention platform for Medicare Advantage health plans.
Here’s what Mia does to keep members engaged:
1. Answers benefit questions on demand: Mia helps members understand what’s covered, what’s not, and what steps to take next, without needing to search for PDFs or sit on hold.
2. Explains plan documents clearly: Members can send in photos of their EOCs, Summary of Benefits, or plan letters, and Mia walks them through what it means in plain terms.
3. Available 24/7: Mia never shuts down. Whether it’s after hours or on weekends, Mia’s ready to help.
4. Supports multiple languages: Members can interact with Mia in the language they’re most comfortable with, without any barriers.
5. Works by voice: Members can ask questions out loud and get clear, verbal responses, without having the need to type.
6. Finds providers fast: Mia helps members find in-network doctors and specialists, based on their location.
7. Clarifies prescriptions in real time: Mia confirms if a medication is covered, what it costs, and whether alternatives exist.
When a member needs support, Mia makes sure they get it- quickly, clearly, and without the usual back-and-forth. When members feel acknowledged and understood, without delay or confusion, they're more likely to trust the plan, use their benefits, and remain loyal to the plan.
Conclusion
Member engagement doesn’t fail because plans don’t care. It fails when members feel like they’re on their own.
Real-time support is how you change that.
Mia is how you make it scalable.
If your goal is to build lasting relationships, don’t just communicate. Connect.
Start with Mia.